Abstract
Background: Living in a disadvantaged neighborhood (reflecting neighborhood-level social determinants of health) is associated with poor health outcomes. BMT survivors remain at a high risk of long-term and late-occurring chronic health conditions that require anticipatory management. We hypothesized that neighborhood disadvantage would be associated with poor health status as reported by the BMT survivors, as well as poor utilization of the healthcare system.
Methods: We leveraged data from BMTSS - a retrospective cohort study examining long-term outcomes among individuals who survived ≥2y following BMT performed at three institutions between 1974 and 2014. Participants in this analysis underwent a single BMT and completed the BMTSS survey, which captures sociodemographic characteristics and chronic health conditions. We graded chronic health conditions using CTCAE v5.0, and calculated a summative index that takes into account the number and grades of the conditions, where a higher score indicates more/worse conditions. The survey also captured self-reported health status ("In general would you say your health is: excellent, very good, good, fair or poor?") and healthcare utilization ("When was your most recent routine check-up? <1y ago, 1-2y ago, 2-5y ago, ≥5y ago, never"). Neighborhood disadvantage was measured using the Area Deprivation Index (ADI), a validated composite indicator based on 17 US Census measures and percentiled as 0 (least deprived) to 100 (most deprived). BMT survivors were linked to ADI via census block group using home address at survey completion. Using multivariable ordered logit regression, we modeled the association between ADI and the odds of worse self-reported health or a longer time since a routine healthcare visit. Models were adjusted for available clinical factors (primary cancer diagnosis, donor source, conditioning intensity, chronic health conditions, chronic graft vs. host disease (GvHD), time from BMT) and individual-level sociodemographic characteristics (age at survey, sex, payor, race/ethnicity, education, income, marital status).
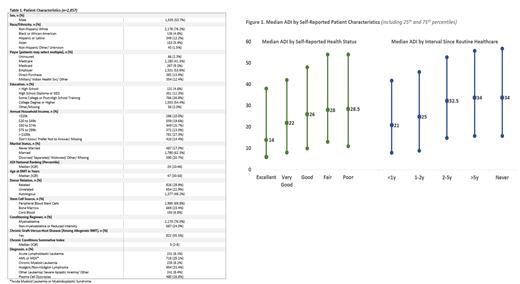
Results: The cohort included 2,893 BMT survivors; median age at BMT was 47y (IQR: 30-58); median follow-up time was 9y (IQR: 5-16). Table 1 summarizes patient characteristics. Median ADI ranged from 14.0 in patients rating their health as excellent to 28.5 in those rating their health as poor, and from 21.0 in patients with visits <1y ago to 34.0 in patients reporting no visits [Fig 1]. In multivariable analyses, the odds of reporting worse health were higher for patients residing in more disadvantaged neighborhoods (OR per_unit_higher_ADI=1.005, p=0.003). Thus, for our cohort, a patient living in the most disadvantaged neighborhood (ADI=100) had 1.65 times the odds of reporting poor health compared to a patient living in the least disadvantaged neighborhood (ADI=1). Further, the odds of a longer time since the last routine physician visit were higher for patients living in more disadvantaged neighborhoods (OR per_unit_higher_ADI=1.007, p<0.001). Thus, a patient living in the most disadvantaged neighborhood had twice the odds (OR=2.06) of reporting no visits compared to a patient living in the least disadvantaged neighborhood.
Conclusions: Conditional on surviving 2 or more years after BMT, living in a disadvantaged neighborhood was associated with poorer self-reported health and a longer time interval since a routine healthcare visit, after adjusting for self-reported individual socioeconomic indicators and chronic health conditions. The significant association between area deprivation and poorer self-reported health persisted after controlling for prior health care utilization. Our findings suggest that health status and access to healthcare are associated with characteristics of the built and social environment and deserve detailed examination in order to inform multi-level interventions that include policy.
Arora: Syndax: Research Funding; Kadmom: Research Funding; Pharmacyclics: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal